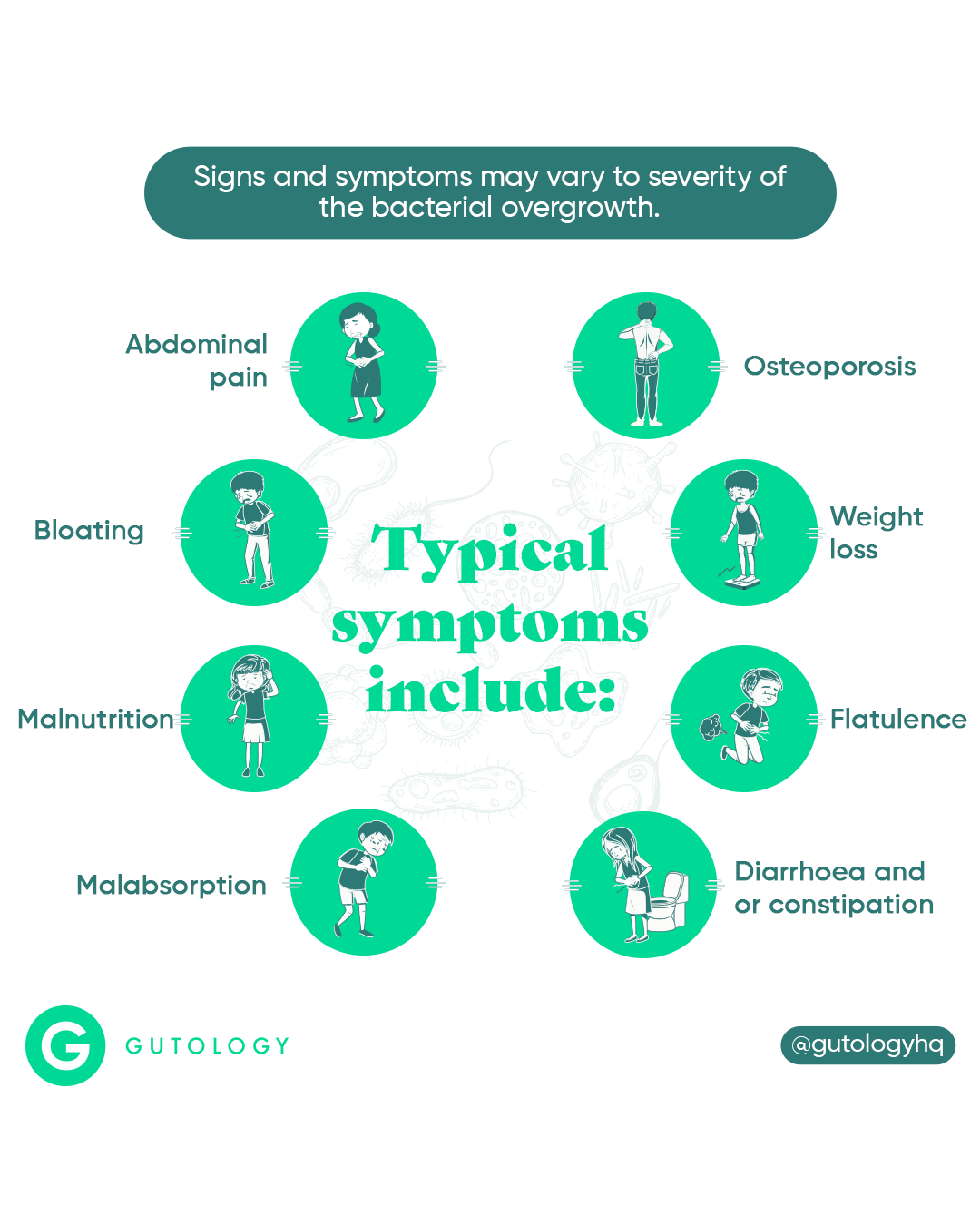
SIBO is a condition in which bacteria normally found in the colon proliferates in large numbers in the small intestine.1 Signs and symptoms may vary due to the type of bacterial overgrowth2 and the severity of disease.3 Typical symptoms tend to overlap with those of IBS, and include bloating, abdominal pain, flatulence, diarrhoea and/or constipation, weight loss, malabsorption, malnutrition and osteoporosis.1,2 Several conditions are also linked with SIBO such as rosacea, hypothyroid, lactose intolerance, coeliac disease, inflammatory bowel disease, chronic fatigue syndrome and fibromyalgia to name a few.
How to fix it
The 5R gut restoration protocol, implemented in the correct sequence, can be effective in managing SIBO:
Remove
Simple sugars and well-absorbed carbohydrates (such as grains, legumes, starchy vegetables) should be eliminated, as they feed the bacteria creating symptoms and fuel more bacterial growth. Reduction of any drugs that reduce intestinal motility or stomach acidity to its lowest possible level is also advised1. Conventionally, antibiotics are used to eradicate SIBO4 but due to potential adverse effects,8 specific strain probiotics (such as Lactobacillus casei and L. acidophilus) can be used as an alternative therapy.8,9
Replace
Insufficient stomach acid, bile and digestive enzymes may be a key factor in SIBO,4 and replacing these through supplementation may be required to decrease ingested bacterial load. Any nutritional deficiencies as a consequence of SIBO (particularly vitamins A, D, E, K and B12, calcium and magnesium)2 will need to be corrected.
Re-inoculate
As a second stage process, once SIBO has been removed, multi-strain probiotics are used to re- establish a healthy gut microflora balance.10
Repair
SIBO can cause inflammation and damage the lining of the small intestine.2 As part of the second stage, gut healing nutrients such as L-glutamine,11 essential fatty acids, zinc and quercetin;12,13 and anti-inflammatory agents such as curcumin and resveratrol14 can be used to repair the gut.
Rebalance
Stress has a negative effect on gut motility, intestinal permeability, gut barrier regeneration, gut flora balance and the immune system.15 Stress management is therefore important in maintaining gut health. In addition, spacing meals 4-5 hours apart will allow the small intestine to clear away bacteria at night and in between meals.16
What causes it?
There are several natural defenses that prevent bacterial overgrowth in the small intestine. Stomach acid, bile and pancreatic juices destroy or limit bacterial growth. Muscular activity of the small intestine work to propel not only food, but also bacteria away and out into the colon. The intestinal mucus layer and the immune system also aid in preventing bacterial proliferation. SIBO can develop if some of these defence mechanisms are disrupted.4
Who's at risk?
Though the following factors do not necessarily lead to SIBO, there is evidence that they lead to an increased risk of developing it:
- Chronic antacid use7
- Recurrent antibiotic use2
- Use of narcotics1
- The elderly2
- Gastrointestinal surgery1
- Those with constipation, IBS, diabetes, coeliac disease, low stomach acid, scleroderma, intestinal diverticulosis, and intestinal obstructions caused by strictures, adhesions and cancer.1,2
Diagnosing SIBO
The most efficient and non-invasive method for testing for SIBO is through a glucose and hydrogen breath test.6 This kind of test can be arranged via our Clinic following a consultation with one of our gutologists.
- Sachdev, A.H. and Pimentel, M., 2013. Gastrointestinal bacterial overgrowth: pathogenesis and clinical significance. Therapeutic advances in chronic disease, 4(5), pp.223-231.
- Dukowicz, A.C., Lacy, B.E. and Levine, G.M., 2007. Small intestinal bacterial overgrowth: a comprehensive review. Gastroenterology & hepatology, 3(2), p.112.
- Grace, E., Shaw, C., Whelan, K. and Andreyev, H.J.N., 2013. small intestinal bacterial overgrowth–prevalence, clinical features, current and developing diagnostic tests, and treatment. Alimentary pharmacology & therapeutics, 38(7), pp.674-688.
- Bures, J., Cyrany, J., Kohoutova, D., Förstl, M., Rejchrt, S., Kvetina, J., Vorisek, V. and Kopacova, M., 2010. Small intestinal bacterial overgrowth syndrome. World journal of gastroenterology: WJG, 16(24), p.2978.
- Franco, D.L., Disbrow, M.B., Kahn, A., Koepke, L.M., Harris, L.A., Harrison, M.E., Crowell, M.D. and Ramirez, F.C., 2015. Duodenal aspirates for small intestine bacterial overgrowth: yield, PPIs, and outcomes after treatment at a tertiary academic medical center. Gastroenterology research and practice, 2015.
- Ghoshal U. C. (2011). How to interpret hydrogen breath tests. Journal of neurogastroenterology and motility, 17(3), 312– 317. doi:10.5056/jnm.2011.17.3.312
- Lo, W.K. and Chan, W.W., 2013. Proton pump inhibitor use and the risk of small intestinal bacterial overgrowth: a meta- analysis. Clinical Gastroenterology and Hepatology, 11(5), pp.483-490.
- Chen, W. C., & Quigley, E. M. (2014). Probiotics, prebiotics & synbiotics in small intestinal bacterial overgrowth: opening up a new therapeutic horizon!. The Indian journal of medical research, 140(5), 582–584.
- Soifer, L.O., Peralta, D., Dima, G. and Besasso, H., 2010. Comparative clinical efficacy of a probiotic vs. an antibiotic in the treatment of patients with intestinal bacterial overgrowth and chronic abdominal functional distension: a pilot study. Acta gastroenterologica Latinoamericana, 40(4), pp.323-327.
- L Madsen, K., 2012. Enhancement of epithelial barrier function by probiotics. Journal of Epithelial Biology and Pharmacology, 5(1).
- Krishna Rao, R. (2012). Role of Glutamine in Protection of Intestinal Epithelial Tight Junctions. Journal of Epithelial Biology and Pharmacology, 5(1), pp.47-54.
- Dulantha Ulluwishewa, Rachel C. Anderson, Warren C. McNabb, Paul J. Moughan, Jerry M. Wells, Nicole C. Roy., 2011. Regulation of Tight Junction Permeability by Intestinal Bacteria and Dietary Components, The Journal of Nutrition, Volume 141, Issue 5, Pages 769–776, https://doi.org/10.3945/jn.110.135657
- Lan, A., Blachier, F., Benamouzig, R., Beaumont, M., Barrat, C., Coelho, D., Lancha Jr, A., Kong, X., Yin, Y., Marie, J.C. and Tomé, D., 2014. Mucosal healing in inflammatory bowel diseases: is there a place for nutritional supplementation?. Inflammatory bowel diseases, 21(1), pp.198-207.
- Bereswill, S., Muñoz, M., Fischer, A., Plickert, R., Haag, L.M., Otto, B., Kühl, A.A., Loddenkemper, C., Göbel, U.B. and Heimesaat, M.M., 2010. Anti-inflammatory effects of resveratrol, curcumin and simvastatin in acute small intestinal inflammation. PloS one, 5(12), p.e15099.
- Konturek, P.C., Brzozowski, T. and Konturek, S.J., 2011. Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. J Physiol Pharmacol, 62(6), pp.591-599.
- Pimentel, M., 2006. A new IBS solution. California, Health Point Press.